General information
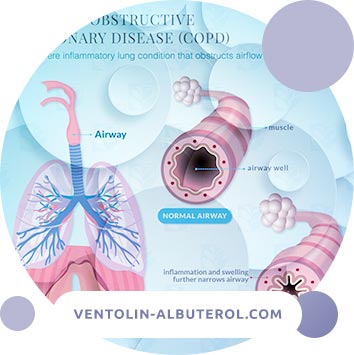
Chronic obstructive pulmonary disease (COPD) is a chronic inflammatory disease that occurs under the influence of various factors of environmental aggression, the main of which is smoking. It proceeds with a predominant lesion of the distal airways and lung parenchyma, the formation of emphysema.
COPD is characterized by a partially reversible and irreversible limitation of air velocity. The disease is caused by an inflammatory reaction that differs from inflammation in bronchial asthma and exists regardless of the severity of the disease.
COPD develops in predisposed individuals and is manifested by cough, sputum production and increasing shortness of breath. The disease has a steadily progressing character with an outcome in chronic respiratory failure and pulmonary heart.
Currently, the concept of "COPD" has ceased to be collective. Partially reversible airflow restriction associated with the presence of bronchiectasis, cystic fibrosis, post-tuberculous fibrosis, bronchial asthma is excluded from the definition of "COPD".
Note. Specific approaches to the treatment of COPD in this section are presented in accordance with the views of the leading pulmonologists of the Russian Federation and may not coincide in detail with the recommendations of GOLD - 2011.
Classification
Classification of the severity of airflow rate limitation in COPD (based on postbronchodilation FEV1) in patients with FEV1 / FVC <0.70 (GOLD - 2011)
| GOLD 1 | Easy | FEV1 ≥80% of due |
| GOLD 2 | Moderate | 50% ≤ FEV1 <80% of due |
| GOLD 3 | Heavy | 30% ≤ FEV1 <50% of due |
| GOLD 4 | Extremely heavy | FEV1 <30% of due |
Clinical classification of COPD by severity (used if it is impossible to dynamically monitor the state of FEV1 / FVC, when the stage of the disease can be approximately determined based on an analysis of clinical symptoms).
Stage I. Mild COPD: the patient may not notice that he has impaired lung function; usually (but not always) chronic cough and sputum production are noted.
Stage II. Moderate course of COPD: at this stage, patients seek medical help due to shortness of breath and exacerbation of the disease. There is an increase in symptoms with shortness of breath that occurs during physical exertion. The presence of repeated exacerbations affects the quality of life of patients and requires appropriate treatment tactics.
Stage III. Severe COPD: characterized by a further increase in airflow restriction, increased shortness of breath, and the frequency of exacerbations of the disease, which affects the quality of life of patients.
Stage IV. Extremely severe COPD: at this stage, the quality of life of patients is markedly deteriorating, and exacerbations can be life threatening. The disease acquires a disabling course. Extremely severe bronchial obstruction in the presence of respiratory failure is characteristic. As a rule, the partial pressure of oxygen in arterial blood (PaO2) is less than 8.0 kPa (60 mm Hg) in combination (with or without) with an increase in PaCO2 over 6.7 kPa (50 mm Hg). Perhaps the development of pulmonary heart.
Note. Stage of severity "0": Increased risk of developing COPD: chronic cough and sputum production; exposure to risk factors, lung function is not changed. This stage is considered as a pre-disease, which does not always turn into COPD. It allows to identify patients at the risk stage and to prevent the further development of the disease. In current guidelines, stage "0" is excluded.
The severity of the condition without spirometry can also be determined and evaluated in dynamics according to some tests and scales. A very high correlation was noted between spirometric indicators and some scales.
Etiology and pathogenesis
COPD develops as a result of the interaction of genetic factors and environmental factors.
Etiology
Environmental factors:
- smoking (active and passive) is the main etiological factor in the development of the disease;
- smoke from burning biofuels for home cooking is an important etiological factor in underdeveloped countries;
- occupational hazards: organic and inorganic dust, chemical agents.
Genetic factors:
- alpha1-antitrypsin deficiency;
- At present, the polymorphism of genes of microsomal epoxy hydrolase, vitamin D-binding protein, MMP12 and other possible genetic factors is being investigated.
Pathogenesis
Airway inflammation in patients with COPD is a pathologically enhanced normal inflammatory response of the airways to long-term irritating factors (such as cigarette smoke). The mechanism for the emergence of an enhanced response is currently not well understood; it is noted that it can be genetically determined. In some cases, the development of COPD in non-smokers is observed, however, the nature of the inflammatory response in these patients is unknown. Due to oxidative stress and an excess of proteinases in the lung tissue, a further increase in the inflammatory process occurs. This together leads to pathomorphological changes characteristic of COPD. The inflammatory process in the lungs continues after smoking cessation. The role of autoimmune processes and persistent infection in the continuation of the inflammatory process is discussed.
Pathophysiology
1. Airflow limitation and "air traps". Inflammation, fibrosis and hyperproduction of exudate in the lumen of the small bronchi cause obstruction. As a result of this, "air traps" arise - an obstacle to the release of air from the lungs into the expiratory phase, and then hyperinflation develops. Emphysema also contributes to the formation of "air traps" on exhalation, although it is more associated with impaired gas exchange than with a decrease in FEV1. Due to hyperinflation, which leads to a decrease in inspiratory volume (especially during physical exertion), shortness of breath and limitation of exercise tolerance appear. These factors cause impaired contractility of the respiratory muscles, which leads to increased synthesis of pro-inflammatory cytokines.
Currently, it is believed that hyperinflation develops already in the early stages of the disease and serves as the main mechanism for the occurrence of shortness of breath during exercise.
2. Gas exchange disorders lead to hypoxemia and hypercapnia, and in COPD are due to several mechanisms. Transport of oxygen and carbon dioxide in general becomes worse as the disease progresses. Severe obstruction and hyperinflation in combination with impaired contractility of the respiratory muscles lead to an increase in the load on the respiratory muscles. Such an increase in load combined with a decrease in ventilation can lead to the accumulation of carbon dioxide. Violation of alveolar ventilation and a decrease in pulmonary blood flow lead to further progression of the violation of the ventilation-perfusion ratio (VA / Q).
3. Hypersecretion of mucus, which leads to a chronic productive cough, is a characteristic feature of chronic bronchitis and is not necessarily combined with limitation of air flow rate. Symptoms of mucus hypersecretion are not detected in all patients with COPD. In the presence of hypersecretion, it is caused by mucosal metaplasia with an increase in the number of goblet cells and the size of the submucous glands, which occurs in response to the chronic irritating effect on the respiratory tract of cigarette smoke and other harmful agents. Hypersecretion of mucus is stimulated by various mediators and proteinases.
4. Pulmonary hypertension may develop in the later stages of COPD. Its appearance is associated with spasm of small arteries of the lungs caused by hypoxia, which ultimately leads to structural changes: intimal hyperplasia and later hypertrophy / hyperplasia of the smooth muscle layer.
In the vessels, endothelial dysfunction and an inflammatory reaction similar to the reaction in the respiratory tract are observed.
Depression of pulmonary capillary blood flow in emphysema can also contribute to increased pressure in the pulmonary circle. Progressive pulmonary hypertension can lead to right ventricular hypertrophy and ultimately to right ventricular failure (pulmonary heart).
5. Exacerbations with increased respiratory symptoms in patients with COPD can be triggered by a bacterial or viral infection (or a combination thereof), environmental pollution and unidentified factors. With a bacterial or viral infection, a characteristic increase in the inflammatory response is observed in patients. During exacerbation, there is an increase in the severity of hyperinflation and "air traps" in combination with a decreased expiratory flow, which leads to increased shortness of breath. In addition, an exacerbation of the imbalance of the ventilation-perfusion ratio (VA / Q), which leads to severe hypoxemia, is revealed.
Such diseases as pneumonia, thromboembolism and acute heart failure can simulate an exacerbation of COPD or aggravate its picture.
6. Systemic manifestations. Limiting air flow and especially hyperinflation negatively affects heart function and gas exchange. The inflammatory mediators circulating in the blood can contribute to the loss of muscle mass and cachexia, and can also provoke the development or aggravate the course of concomitant diseases (coronary heart disease, heart failure, normocytic anemia, osteoporosis, diabetes, metabolic syndrome, depression).
Pathomorphology
In the proximal airways, peripheral airways, lung parenchyma and pulmonary vessels with COPD characteristic pathomorphological changes are found:
- Signs of chronic inflammation with an increase in the number of specific types of inflammatory cells in different parts of the lungs;
- structural changes due to the alternation of damage and repair processes.
As COPD increases in severity, inflammatory and structural changes increase and persist even after quitting smoking.
Epidemiology
Existing data on the prevalence of COPD have significant differences (from 8 to 19%), due to differences in research methods, diagnostic criteria and approaches to data analysis. On average, prevalence is estimated at about 10% in a population.
Factors and risk groups
- smoking (active and passive) is the main and main risk factor; smoking during pregnancy can put the fetus at risk through harmful effects on intrauterine growth and lung development and, possibly, through primary antigenic effects on the immune system;
- genetic congenital deficiencies of certain enzymes and proteins (most often antitrypsin deficiency);
- occupational hazards (organic and inorganic dust, chemical agents and smoke);
- male gender;
- age over 40 (35) years;
- socio-economic status (poverty);
- low body weight;
- low body weight at birth, as well as any factor that has an adverse effect on lung growth during fetal development and in childhood;
- bronchial hyperreactivity;
- chronic bronchitis (especially in young smokers);
- Severe respiratory infections from childhood.
Clinical picture
Symptoms, course
In the presence of cough, sputum production and / or shortness of breath, COPD should be assumed in all patients with risk factors for the development of the disease. It should be borne in mind that chronic cough and sputum production can often occur long before the development of airflow restriction, which leads to shortness of breath.
If the patient has any of these symptoms, spirometry must be performed. Each symptom individually is not diagnostic, but the presence of several of them increases the likelihood of having COPD.
Diagnosis of COPD consists of the following steps:
- information gleaned from a conversation with the patient (verbal portrait of the patient);
- data of an objective (physical) examination;
- the results of instrumental laboratory research.
The study of the verbal portrait of the patient
Complaints (their severity depends on the stage and phase of the disease):
1. Cough is the earliest symptom and usually occurs between the ages of 40-50. In the cold seasons, such patients experience episodes of a respiratory infection, which at first are not associated by the patient and the doctor in one disease. Coughing may be daily or intermittent; more commonly observed during the day.
In a conversation with the patient, it is necessary to establish the frequency of coughing and its intensity.
2. Sputum, as a rule, is excreted in a small amount in the morning (rarely> 50 ml / day), has a mucous character. An increase in the amount of sputum and its purulent nature are signs of an exacerbation of the disease. If blood appears in sputum, another cause of cough should be suspected (lung cancer, tuberculosis, bronchiectasis). In a patient with COPD, streaks of blood in the sputum can appear as a result of a persistent nasal cough.
In a conversation with the patient, it is necessary to find out the nature of sputum and its quantity.
3. Shortness of breath is the main symptom of COPD and for most patients is an occasion to see a doctor. Often, the diagnosis of COPD is established at this stage of the disease.
As the disease progresses, dyspnea can vary widely: from a feeling of lack of air during normal physical exertion to severe respiratory failure. Dyspnea during physical exertion appears on average 10 years later than coughing (extremely rarely the disease debuts shortness of breath). The severity of dyspnea increases with a decrease in pulmonary function.
In COPD, the characteristic features of shortness of breath are:
- progression (continuous increase);
- constancy (every day);
- gain during exercise;
- increase in respiratory infections.
Patients describe shortness of breath as "increased effort during breathing," "heaviness," "air starvation," "shortness of breath."
In a conversation with the patient, it is necessary to assess the severity of shortness of breath and its relationship with physical activity. There are several special scales for assessing dyspnea and other symptoms of COPD - BORG, mMRC Dyspnea Scale, CAT.
Along with the main complaints, patients may be disturbed by the following extrapulmonary manifestations of COPD:
- morning headache;
- drowsiness during the day and insomnia at night (a consequence of hypoxia and hypercapnia);
- weight loss and weight loss.
Anamnesis
When talking with a patient, it should be borne in mind that COPD begins to develop long before the onset of severe symptoms and for a long time proceeds without vivid clinical symptoms. It is desirable for the patient to clarify with what he himself associates the development of the symptoms of the disease and their increase.
When studying the anamnesis, it is necessary to establish the frequency, duration and characteristics of the main manifestations of exacerbations and evaluate the effectiveness of previous treatment measures. It is required to find out the presence of a hereditary predisposition to COPD and other pulmonary diseases.
If the patient underestimates his condition and the doctor has difficulty determining the nature and severity of the disease, special questionnaires are used.
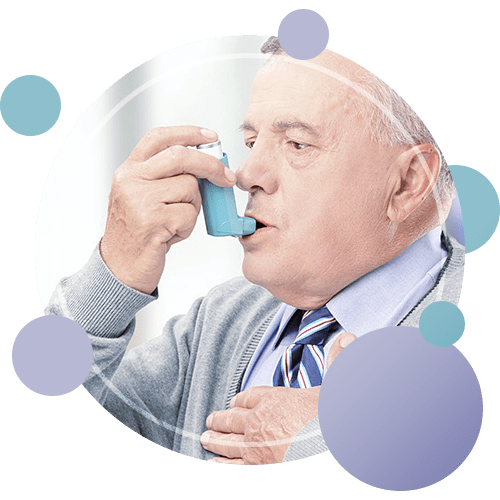
Typical "portrait" of a patient with COPD:
- smoker;
- middle or old age;
- suffering from shortness of breath;
- having a chronic cough with sputum, especially in the morning;
- complaining of regular exacerbations of bronchitis;
- having partially (slightly) reversible obstruction.
Physical examination
The results of an objective examination depend on the following factors:
- the severity of bronchial obstruction;
- severity of emphysema;
- the presence of manifestations of pulmonary hyperinflation (pulmonary distension);
- the presence of complications (respiratory failure, chronic pulmonary heart);
- the presence of concomitant diseases.
It should be borne in mind that the absence of clinical symptoms does not exclude the presence of COPD in the patient.
Patient examination
1. Assessment of the patient's appearance, his behavior, the reaction of the respiratory system to conversation, movement in the office. Signs of a severe course of COPD are collected lips and a forced position.
2. Assessment of skin coloration, which is determined by a combination of hypoxia, hypercapnia and erythrocytosis. Central gray cyanosis usually serves as a manifestation of hypoxemia; if it is combined with acrocyanosis, then this usually indicates the presence of heart failure.
3. Inspection of the chest. Signs of severe COPD:
- chest deformity, "barrel-shaped" form;
- inactive while breathing;
- paradoxical retraction (retraction) of the lower intercostal spaces on inspiration (sign of Hoover);
- participation in the act of breathing of the auxiliary muscles of the chest, abdominal press;
- significant expansion of the chest in the lower parts.
4. Chest percussion. Signs of emphysema are a boxed percussion sound and lowered lower boundaries of the lungs.
5. Auscultatory picture:
- Signs of emphysema: hard or weakened vesicular breathing in combination with a low standing of the diaphragm;
- obstruction syndrome: dry wheezing, which intensifies with forced expiration, in combination with increased expiration.
Clinical forms of COPD
In patients with moderate to severe disease, two clinical forms are distinguished:
- emphysematous (panacinar emphysema, "pink puff");
- bronchitis (centroacinar emphysema, "blue edema").
Isolation of two forms of COPD is predictive. With the emphysematous form, decompensation of the pulmonary heart occurs in later stages compared to the bronchitis form. Often there is a combination of these two forms of the disease.
According to clinical signs, two main phases of the course of COPD are distinguished: stable and exacerbation of the disease.
A stable state - the progression of the disease can be detected only with prolonged dynamic monitoring of the patient, and the severity of symptoms does not change significantly for weeks or even months.
An exacerbation is a worsening of the patient's condition, which is accompanied by an increase in symptoms and functional disorders and lasts at least 5 days. Exacerbations can have a gradual onset or manifest a rapid deterioration in the patient's condition with the development of acute respiratory and right ventricular failure.
The main symptom of exacerbation of COPD is increased shortness of breath. As a rule, this symptom is accompanied by a decrease in exercise tolerance, a feeling of constriction in the chest, the occurrence or intensification of distance rales, an increase in the intensity of coughing and the amount of sputum, and a change in its color and viscosity. In patients, the indicators of the function of external respiration and blood gases are significantly worsened: speed indicators (OFV1, etc.) are reduced, the appearance of hypoxemia and hypercapnia is possible.
There are two types of exacerbation:
- an exacerbation characterized by an inflammatory syndrome (fever, increase in the number and viscosity of sputum, purulent sputum);
- exacerbation, manifested by an increase in shortness of breath, increased extrapulmonary manifestations of COPD (weakness, headache, poor sleep, depression).
There are 3 degrees of severity of exacerbation, depending on the intensity of the symptoms and the response to treatment:
- Mild - the symptoms are slightly increased, the exacerbation is stopped with the help of bronchodilator therapy.
- Moderate - exacerbation requires medical intervention and can be stopped on an outpatient basis.
- Severe - exacerbation requires inpatient treatment, characterized by increased symptoms of COPD and the appearance or worsening of complications.
In patients with mild or moderate COPD (stage I – II), exacerbation is usually manifested by increased shortness of breath, cough and increased sputum volume, which allows patients to be treated on an outpatient basis.
In patients with severe COPD (stage III), exacerbations are often accompanied by the development of acute respiratory failure, which requires intensive care in an inpatient setting.
In some cases, in addition to severe, very severe and extremely severe exacerbations of COPD are distinguished. In these situations, participation in the act of breathing of the auxiliary muscles, paradoxical movements of the chest, the occurrence or exacerbation of central cyanosis and peripheral edema are taken into account.
Diagnostics
Instrumental research
1. The study of the function of external respiration is the main and most important method for diagnosing COPD. It is used to detect airflow restriction in patients with chronic productive cough, even in the absence of shortness of breath.
The main functional syndromes in COPD:
- violation of bronchial patency;
- a change in the structure of static volumes, a violation of the elastic properties and diffusion ability of the lungs;
- decreased physical performance.
Spirometry
Spirometry or pneumotachometry are common methods for recording bronchial obstruction. When conducting research, evaluate forced expiration in the first second (FEV1) and forced vital lung capacity (FVC).
The presence of chronic airflow restriction or chronic obstruction is indicated by a post-bronchodilatory decrease in the FEV1 / FVC ratio of less than 70% of the proper value. This change is recorded starting from stage I of the disease (mild COPD).
The postbronchodilation indicator OFV1 has a high degree of reproducibility with the correct execution of maneuver and allows you to monitor the condition of bronchial patency and its variability.
Bronchial obstruction is considered chronic if it is recorded at least 3 times in one year, despite ongoing therapy.
Bronchodilation test is carried out:
- with short-acting β2-agonists (inhalation of 400 μg of salbutamol or 400 μg of phenoterol), the assessment is carried out after 30 minutes;
- with M-anticholinergics (inhalation of ipratropium bromide 80 mcg), evaluation is carried out after 45 minutes;
- it is possible to conduct a test with a combination of bronchodilators (phenoterol 50 μg + ipratropium bromide 20 μg - 4 doses).
To correctly perform the bronchodilation test and avoid distortion of the results, it is necessary to cancel the therapy in accordance with the pharmacokinetic properties of the drug taken:
- β2-agonists of short action - 6 hours before the start of the test;
- long-acting β2-agonists - in 12 hours;
- prolonged theophyllines - in 24 hours.
Calculation of growth OFV1
- Measurement of bronchodilation response by the absolute increase in OFB1 in ml (the easiest way): Disadvantage: this method does not allow us to judge the degree of relative improvement in bronchial patency, since neither the initial nor the achieved indicator is taken into account in relation to what is due.
- A method for measuring reversibility by the percentage of the absolute increase in the FEV1 indicator to the initial FEV1: Disadvantage: a slight absolute increase will ultimately give a high percentage increase if the patient has an initially low FEV1 indicator.
- A method for measuring the degree of bronchodilation response as a percentage in relation to due OFB1 [ΔOFB1 due. (%)].
- A method for measuring the degree of bronchodilation response as a percentage of the maximum possible reversibility [ΔOФВ1 prob. (%)]: where OFB1 ref. - initial parameter, OFV1 dilat. - indicator after bronchodilation test, OFV1 due. - due parameter.
The choice of method for calculating the reversibility index depends on the clinical situation and the specific reason in connection with which the study is being conducted. The use of the reversibility index, which is less dependent on the initial parameters, allows for a more correct comparative analysis.
In most cases, a method for calculating growth relative to the proper FEV1 values is recommended.
The marker of a positive bronchodilation response is considered to be the increase in OFV1 ≥15% of the due and ≥ 200 ml. Upon receipt of such an increase, bronchial obstruction is documented as reversible.
Bronchial obstruction can lead to a change in the structure of static volumes in the direction of pulmonary hyperair, a manifestation of which, in particular, is an increase in the total lung capacity.
To detect changes in the ratios of static volumes that make up the structure of the total capacity of the lungs with hyperair and emphysema, bodyplethysmography and measurement of pulmonary volumes by the method of inert gas dilution are used.
Bodyplethysmography
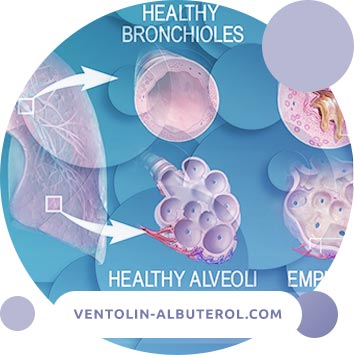
With emphysema, the anatomical changes in the lung parenchyma (expansion of air spaces, destructive changes in the alveolar walls) are functionally manifested by an increase in the static extensibility of the lung tissue. A change in the shape and angle of the pressure-volume loop is noted.
Measurement of the diffusion ability of the lungs is used to detect damage to the pulmonary parenchyma due to emphysema and is performed after forced spirometry or pneumotachometry and determination of the structure of static volumes.
In emphysema, lung diffusion capacity (DLCO) and its relation to the alveolar volume of DLCO / Va are reduced (mainly as a result of destruction of the alveolar-capillary membrane, which reduces the effective gas exchange area).
It should be borne in mind that a decrease in the diffusion capacity of the lungs per unit volume can be compensated by an increase in the total capacity of the lungs.
Peak flowmetry
Determining the volume of peak expiratory flow rate (PSV) is the simplest fast-performing method for assessing the state of bronchial obstruction. However, it has low sensitivity, since with COPD, PSV values can remain within normal limits for a long time, and low specificity, since a decrease in PSV values can also be with other respiratory diseases.
Peak flowmetry is used in the differential diagnosis of COPD and bronchial asthma, and can also be used as an effective screening method to identify risk groups for developing COPD and to establish the negative impact of various pollutants.
Determination of PSV is a necessary control method during a period of exacerbation of COPD and especially at the rehabilitation stage.
2. Chest x-ray.
An initial X-ray examination is carried out to exclude other diseases (lung cancer, tuberculosis, etc.), accompanied by clinical symptoms similar to COPD.
With a mild COPD, significant radiological changes, as a rule, are not detected.
With exacerbation of COPD, an X-ray examination is performed to exclude the development of complications (pneumonia, spontaneous pneumothorax, pleural effusion).
X-ray of the chest organs reveals emphysema. An increase in lung volume is indicated by:
- on a direct radiograph - a flat diaphragm and a narrow shadow of the heart;
- on the lateral radiograph - flattening of the diaphragmatic contour and an increase in retrosternal space.
Confirmation of the presence of emphysema can be the presence of bullae on the radiograph - defined as radiolucent spaces more than 1 cm in diameter with a very thin arcuate border.
3. Computed tomography of the chest is required in the following situations:
- when the existing symptoms are disproportionate to spirometric data;
- to clarify the changes identified during chest x-ray;
- to evaluate indications for surgical treatment.
CT, especially of high resolution (CTEC) with a pitch of 1 to 2 mm, has a higher sensitivity and specificity for the diagnosis of emphysema compared to radiography. Using CT in the early stages of development, it is also possible to identify the specific anatomical type of emphysema (panacinar, centroacinar, paraseptal).
With CT in many patients with COPD, saber-shaped tracheal deformity pathognomonic for this disease is detected.
Since a standard CT scan is performed at the height of the inspiration, when the excess airiness of the lung tissue is not visible, with suspected COPD, CT scan should be supplemented with expiratory tomography.
CTTV allows you to evaluate the fine structure of the lung tissue and the condition of the small bronchi. The state of lung tissue in case of ventilation disorders in patients with obstructive changes is studied under conditions of expiratory CT. When using this technique, CTEC is performed at the height of the delayed expiration.
In areas of impaired bronchial patency, areas of increased airiness are identified - "air traps" that lead to hyperinflation. This phenomenon occurs as a result of increased lung compliance and a decrease in their elastic traction. During exhalation, airway obstruction causes air retention in the lungs due to the patient's inability to exhale fully.
The indicators of the "air trap" (type IC - inspiratory capacity, inspiratory capacity) are more closely correlated with the state of the respiratory tract of a patient with COPD than the FEV1 indicator.
Other studies
1. In most cases, electrocardiography eliminates the cardiac origin of respiratory symptoms. In some cases, the ECG reveals signs of hypertrophy of the right heart during the development of pulmonary heart disease as a complication of COPD.
2. Echocardiography allows you to evaluate and identify signs of pulmonary hypertension, dysfunction of the right (and, if there are changes, left) parts of the heart and determine the severity of pulmonary hypertension.
3. Study with physical activity (step test). In the initial stages of the disease, violations of the diffusion ability and the gas composition of the blood may be absent at rest and appear only during physical exertion. Exercise testing is recommended to objectify and document the degree to which exercise tolerance is reduced.
A test with physical activity is carried out in the following cases:
- when the severity of shortness of breath does not correspond to a decrease in the FEV1 values;
- to monitor the effectiveness of the therapy;
- for the selection of patients for rehabilitation programs.
The most commonly used step test is a 6-minute walk test, which can be performed on an outpatient basis and is the easiest way to individually monitor and monitor the course of the disease.
The standard test protocol with a 6-minute walk includes instructing patients on the goals of the test, then they are invited to walk along the measured corridor at their own pace, trying to cover the maximum distance for 6 minutes. Patients are allowed to stop and rest during the test, resuming walking after rest.
Before and at the end of the test, dyspnea is assessed according to the Borg scale (0-10 points: 0 - no dyspnea, 10 - maximum dyspnea), SatO2 and pulse. Patients stop walking when they experience severe shortness of breath, dizziness, pain in the chest or legs, with a decrease in SatO2 of 86%. The distance covered in 6 minutes is measured in meters (6MWD) and compared with the proper indicator 6MWD (i).
The 6-minute walk test is part of the BODE scale (see the "Forecast" section), which allows you to compare the FEV1 values with the mMRC scale and body mass index.
4. A bronchoscopic examination is used in the differential diagnosis of COPD with other diseases (cancer, tuberculosis, etc.), manifested by similar respiratory symptoms. The study includes examination of the mucous membrane of the bronchi and assessment of its condition, taking bronchial contents for subsequent studies (microbiological, mycological, cytological).
If necessary, it is possible to conduct a biopsy of the mucous membrane of the bronchi and the technique of bronchoalveolar lavage with the determination of the cellular and microbial composition in order to clarify the nature of the inflammation.
5. The study of quality of life. Quality of life is an integral indicator that determines the patient's adaptation to COPD. To determine the quality of life, special questionnaires are used (non-specific questionnaire SF-36). The most famous St. George hospital questionnaire is The St. George's Hospital Respiratory Questionnaire - SGRQ.
6. Pulse oximetry is used to measure and monitor SatO2. It allows you to record only the level of oxygenation and does not allow you to monitor changes in PaCO2. If SatO2 is less than 94%, then a study of blood gases is indicated.
Pulse oximetry is indicated to determine the need for oxygen therapy (if there is cyanosis or pulmonary heart or FEV1 <50% of the proper values).
In the formulation of the diagnosis of COPD indicate:
- severity of the course of the disease: mild course (stage I), moderate course (stage II), severe course (stage III) and extremely severe course (stage IV), exacerbation or stable course of the disease;
- the presence of complications (pulmonary heart, respiratory failure, circulatory failure);
- risk factors and smoking index;
- in severe cases of the disease, it is recommended to indicate the clinical form of COPD (emphysema, bronchitis, mixed).
Laboratory diagnostics
1. A study of the gas composition of the blood is carried out for patients with increased dyspnea, a decrease in FEV1 values of less than 50% of the due, to patients with clinical signs of respiratory failure or insufficiency of the right heart.
The criterion of respiratory failure (when breathing air at sea level) is PaO2 less than 8.0 kPa (less than 60 mm Hg), regardless of the increase in PaCO2. Sampling for analysis is preferable to carry out by puncture method of the artery.
2. Clinical blood test:
- with exacerbation: neutrophilic leukocytosis with stab shift and an increase in ESR;
- with a stable course of COPD, there are no significant changes in the content of leukocytes;
- with the development of hypoxemia, a polycythemic syndrome is observed (an increase in the number of red blood cells, a high level of Hb, a low ESR, an increase in hematocrit> 47% in women and> 52% in men, increased blood viscosity);
- detected anemia can cause the occurrence or intensification of shortness of breath.
3. An immunogram is performed to detect signs of immune deficiency in the steady progression of COPD.
4. A coagulogram is performed with polycythemia to select adequate disaggregation therapy.
5. Sputum cytology is performed to identify the inflammatory process and its severity, as well as to identify atypical cells (given the advanced age of most patients with COPD, oncological alertness is always present).
If sputum is absent, the method of studying induced sputum, i.e. collected after inhalation of a hypertonic solution of sodium chloride. The study of sputum smears when stained by Gram allows an indicative identification of the group affiliation (gram-positive, gram-negative) of the pathogen.
6. A sputum culture test is performed to identify microorganisms and select rational antibiotic therapy in the presence of persistent or purulent sputum.
Differential diagnosis
The main disease with which it is necessary to differentiate COPD is bronchial asthma.
The main criteria for the differential diagnosis of COPD and bronchial asthma
| Signs | COPD | Bronchial asthma |
| Age of onset of the disease | Generally older than 35-40 years | More often childish and young |
| History of smoking | Characteristically | Uncharacteristic |
| Extrapulmonary Allergy | Uncharacteristic | Are characteristic |
| Symptoms (cough and shortness of breath) | Constant, progressing slowly | Clinical variability, appear paroxysmal: during the day, day by day, seasonally |
| Overweight Asthma | Uncharacteristic | Characteristic |
| Bronchial obstruction | Not reversible or irreversible | Reversible |
| PSV diurnal variability | <10% | >20% |
| Bronchodilator test | Negative | Positive |
| Pulmonary heart disease | Typically severe | Uncharacteristic |
| Type of inflammation | Prevailing neutrophils, an increase in macrophages (++), an increase in CD8 + T-lymphocytes | Eosinophils, increased macrophages (+), increased CD + Th2 lymphocytes, mast cell activation predominate |
| Inflammatory mediators | Leukotriene B, interleukin 8, tumor necrosis factor | Leukotriene D, interleukins 4, 5, 13 |
| The effectiveness of corticosteroids therapy | Low | High |
The following signs identifying bronchial asthma can help in doubtful cases of diagnosing COPD and asthma:
1. An increase in FEV1 by more than 400 ml in response to inhalation with a short-acting bronchodilator or an increase in FEV1 by more than 400 ml after 2 weeks of treatment with prednisone 30 mg / day for 2 weeks (in patients with COPD, FEV1 and FEV1 / FVC as a result treatment do not reach normal values).
2. Reversibility of bronchial obstruction is the most important differential diagnostic sign. It is known that in patients with COPD after taking a bronchodilator, the increase in FEV1 is less than 12% (and ≤200 ml) from the initial one, and in patients with bronchial asthma, FEV1 usually exceeds 15% (and> 200 ml).
3. About 10% of patients with COPD also have signs of bronchial hyperreactivity.
Other diseases
1. Heart failure. Signs:
- wheezing in the lower parts of the lungs - with auscultation;
- a significant decrease in the ejection fraction of the left ventricle;
- dilatation of the heart;
- expansion of the contours of the heart, congestion (up to pulmonary edema) - on the radiograph;
- restrictive disorders without air flow restriction - in the study of lung function.
2. Bronchiectasis. Signs:
- large volumes of purulent sputum;
- Frequent association with bacterial infection;
- Coarse moist rales of various sizes - with auscultation;
- a symptom of "drumsticks" (bulbous thickening of the terminal phalanges of the fingers and toes);
- expansion of the bronchi and thickening of their walls - on an x-ray or CT.
3. Tuberculosis. Signs:
- starts at any age;
- infiltration in the lungs or focal lesions - with x-ray;
- high incidence in this region.
If pulmonary tuberculosis is suspected, the following are required:
- tomography and / or CT of the lungs;
- sputum microscopy and culture of Mycobacterium tuberculosis, including flotation;
- study of pleural exudate;
- diagnostic bronchoscopy with biopsy for suspected bronchial tuberculosis;
- Mantoux test.
4. Obliterating bronchiolitis. Signs:
- development at a young age;
- no connection with smoking has been established;
- contact with fumes, smoke;
- foci of reduced density during exhalation - with CT;
- Rheumatoid arthritis is often present.
Complications
- acute or chronic respiratory failure;
- secondary polycythemia;
- chronic pulmonary heart;
- pneumonia;
- spontaneous pneumothorax;
- pneumomediastinum.
Treatment
The goals of treatment:
- prevention of disease progression;
- relief of symptoms;
- increased tolerance to physical activity;
- improving the quality of life;
- prevention and treatment of complications;
- prevention of exacerbations;
- reduction in mortality.
The main directions of treatment:
- reduction of the influence of risk factors;
- educational programs;
- treatment of COPD in a stable condition;
- treatment of exacerbation of the disease.
Reducing the impact of risk factors
Smoking cessation is the first mandatory step in the program for the treatment of COPD, as well as the only most effective way to reduce the risk of developing COPD and prevent the progression of the disease.
Guidelines for the treatment of tobacco dependence contain 3 programs:
- A long-term treatment program with the goal of completely giving up smoking - is intended for patients with a strong desire to quit smoking.
- A short treatment program to reduce smoking and increase motivation to quit smoking.
- The program to reduce the intensity of smoking, designed for patients who do not want to quit smoking, but are willing to reduce its intensity.
Industrial hazards, atmospheric and home pollutants
Primary preventive measures are to eliminate or reduce the impact of various pathogenic substances in the workplace. Secondary prevention is equally important - epidemiological control and early detection of COPD.
Educational programs
Education plays an important role in the treatment of COPD, especially in educating patients to stop smoking.
Highlights of educational programs for COPD:
- Patients should understand the nature of the disease, be aware of the risk factors leading to its progression.
- Training should be adapted to the needs and environment of a particular patient, as well as meet the intellectual and social level of the patient and those who care for him.
- The following information is recommended to be included in training programs: smoking cessation; basic information about COPD; general approaches to therapy, specific treatment issues; self-knowledge skills and decision-making during exacerbation.
Treatment of patients with COPD in stable condition
Drug therapy
Bronchodilators are the basis of symptomatic treatment of COPD. All categories of bronchodilators increase exercise tolerance even in the absence of changes in FEV1. Inhalation therapy is preferred.
At all stages of COPD, risk factors must be excluded, annual vaccination with influenza vaccine and short-acting bronchodilators required.
Short-acting bronchodilators are used in patients with COPD as empirical therapy to reduce the severity of symptoms and to limit physical activity. Usually they are used every 4-6 hours. With COPD, the regular use of short-acting β2-agonists is not recommended as monotherapy.
Long-acting bronchodilators or their combination with short-acting β2-agonists and short-acting anticholinergics are prescribed for patients who have symptoms of the disease, despite monotherapy with short-acting bronchodilators.
General principles of pharmacotherapy
1. With mild (stage I) COPD and the absence of clinical manifestations of the disease, regular drug therapy is not required.
2. Patients with intermittent symptoms of the disease are shown inhaled β2-agonists or short-acting M-anticholinergics, which are used on demand.
3. If inhaled bronchodilators are not available, sustained-release theophyllines may be recommended.
4. Anticholinergic drugs are considered the first choice for moderate, severe and extremely severe COPD.
5. M-anticholinergic short-acting (ipratropium bromide) has a longer bronchodilator effect compared with short-acting β2-agonists.
6. According to studies, the use of tiotropium bromide is effective and safe in the treatment of patients with COPD. It was shown that taking tiotropium bromide once a day (compared with salmeterol 2p. / Day) leads to a more pronounced improvement in lung function and a decrease in shortness of breath.
Tiotropia bromide reduces the frequency of exacerbations of COPD with annual use compared with placebo and ipratropium bromide and with 6-month use compared with salmeterol.
Thus, tiotropium bromide, used once a day, seems to be the best basis for the combined treatment of stage II – IV COPD.
7. Xanthines are effective for COPD, but are second-line drugs because of their potential toxicity. In more severe cases of the disease, xanthines can be added to regular inhalation bronchodilator therapy.
8. With a stable course of COPD, it is more effective to use a combination of anticholinergics with short-acting β2-agonists or long-acting β2-agonists.
Nebulizer therapy with bronchodilators is indicated for patients with stage III and IV COPD. To clarify the indications for nebulizer therapy, PSV is monitored for 2 weeks of treatment; therapy continues even with an improvement in peak expiratory flow rate.
9. If bronchial asthma is suspected, a trial treatment with inhaled corticosteroids is performed.
The effectiveness of GCS in COPD is lower than in bronchial asthma, and therefore their use is limited. Long-term treatment with inhaled corticosteroids in patients with COPD is prescribed in addition to bronchodilator therapy in the following cases:
- if the patient has a significant increase in FEV1 in response to this treatment;
- in severe / extremely severe COPD and frequent exacerbations (3 times or more over the past 3 years);
- regular (permanent) treatment with inhaled GCS is indicated for patients with stage III and IV COPD with repeated exacerbations of the disease requiring antibiotics or oral GCS at least once a year.
When the use of inhaled GCS is limited for economic reasons, it is possible to prescribe a course of systemic GCS (no longer than 2 weeks) to identify patients with a pronounced spirometric response.
Systemic GCS with a stable course of COPD is not recommended.
Treatment regimen for bronchodilators at various stages of COPD without exacerbation
1. At the easy stage (I): treatment with bronchodilators is not shown.
2. In moderate (II), severe (III) and extremely severe (IV) stages:
- regular intake of short-acting M-anticholinergics or
- regular use of long-acting M-anticholinergics or
- regular administration of long-acting β2-agonists or
- regular administration of short-acting or long-acting M-anticholinergics + inhaled short-acting or long-acting β2-agonists; or
- regular use of long-acting M-anticholinergics + long-acting theophyllines or
- long-acting inhaled β2-agonists + long-acting theophyllines or
- regular administration of short-acting or long-acting M-anticholinergics + inhaled short-acting or long-acting β2-agonists + theophyllines
Examples of treatment regimens at various stages of COPD without exacerbation
All stages (I, II, III, IV)
1. Exclusion of risk factors.
2. Annual vaccination with influenza vaccine.
3. If necessary, inhalation of one of the following drugs:
- salbutamol (200-400 mcg);
- fenoterol (200-400 mcg);
- ipratropium bromide (40 mcg);
- a fixed combination of phenoterol and ipratropium bromide (2 doses).
Stage II, III, IV
Regular inhalation:
- ipratropium bromide 40 mcg 4 p. / day. or
- tiotropium bromide 18 mcg 1 p. / day. or
- salmeterol 50 mcg 2 r. / day. or
- formoterol "Turbuhaler" 4.5-9.0 mcg or
- Formoterol "Autohaler" 12-24 mcg 2 p. / day. or
- a fixed combination of phenoterol + ipratropium bromide 2 doses of 4 r. / Day. or
- ipratropium bromide 40 mcg 4 p. / day. or tiotropium bromide 18 mcg 1 r. / Day. + salmeterol 50 mcg 2 r. / day. (or Formoterol Turbuhaler 4.5–9.0 μg or Formoterol Autohaler 12-24 μg 2 r. / day or ipratropium bromide 40 μg 4 r. / day.) or
- tiotropium bromide 18 mcg 1 r. / day + inside theophylline 0.2-0.3 g 2 r. / day. or (salmeterol 50 mcg 2 r./day or formoterol Turbuhaler 4.5-9.0 mcg) or
- Ormoterol "Autohaler" 12-24 mcg 2 p. / day. + inside theophylline 0.2-0.3 g 2 p. / day. or ipratropium bromide 40 mcg 4 r. / Day. or
- tiotropium bromide 18 mcg 1 p. / day. + salmeterol 50 mcg 2 r. / day. or formoterol Turbuhaler 4.5-9.0 mcg or
- Formoterol "Autohaler" 12-24 mcg 2 p. / day. + Inside theophylline 0.2-0.3 g 2 p. / day.
Stage III and IV:
- beclomethasone 1000-1500 mcg / day. or budesonide 800-1200 mcg / day. or
- fluticasone propionate 500-1000 mcg / day. - with repeated exacerbations of the disease, requiring at least 1 time per year antibiotics or oral corticosteroids
- a fixed combination of salmeterol 25-50 mcg + fluticasone propionate 250 mcg (1-2 doses 2 r. / day) or formoterol 4.5 mcg + budesonide 160 mcg (2-4 doses 2 r. / day.) the same indications as for inhaled corticosteroids.
As the course of the disease worsens, the effectiveness of drug therapy decreases.
Oxygen therapy
The main cause of death in patients with COPD is acute respiratory failure. In this regard, the correction of hypoxemia using oxygen is the most justified method of treating severe respiratory failure.
In patients with chronic hypoxemia, prolonged oxygen therapy (VCT) is used, which helps to reduce mortality.
VCT is indicated for patients with severe COPD if the possibilities of drug therapy are exhausted and the maximum possible therapy does not lead to an increase in O2 above the boundary values.
The purpose of VCT is to increase PaO2 to not less than 60 mm Hg. at rest and / or SatO2 - not less than 90%. VCT is not indicated for patients with moderate hypoxemia (PaO2> 60 mmHg). Indications for VCT should be based on gas exchange parameters, which were evaluated only during the stable state of patients (3-4 weeks after exacerbation of COPD).
Indications for continuous oxygen therapy:
- PaO2 <55 mm Hg or SatO2 <88% at rest;
- RaO2 - 56–59 mm Hg or SatO2 - 89% in the presence of chronic pulmonary heart and / or erythrocytosis (hematocrit> 55%).
Indications for "situational" oxygen therapy:
- decrease in PaO2 <55 mm Hg or SatO2 <88% during exercise;
- decrease in PaO2 <55 mm Hg or SatO2 <88% during sleep.
Assignment Modes:
- O2 flow 1–2 l / min. - for most patients;
- up to 4-5 l / min. - for the most severe patients.
At night, during exercise and during air travel, patients should increase the oxygen flow by an average of 1 l / min. compared to the optimal daily flow.
According to international studies by MRC and NOTT (from nocturnal oxygen therapy), VCT is recommended for at least 15 hours / day. with interruptions not exceeding 2 consecutive hours.
Possible side effects of oxygen therapy:
- violation of mucociliary clearance;
- decrease in cardiac output;
- decrease in minute ventilation, carbon dioxide delays;
- systemic vasoconstriction;
- pulmonary fibrosis.
Long-term mechanical ventilation
Non-invasive ventilation is carried out using a mask. It helps to improve the gas composition of arterial blood, shorten hospitalization days and improve the quality of life of patients.
Indications for prolonged mechanical ventilation in patients with COPD:
- PaCO2> 55 mm Hg;
- PaCO2 in the range of 50–54 mm Hg in combination with night desaturation and frequent episodes of hospitalization of the patient;
- shortness of breath at rest (respiratory rate> 25 per minute);
- participation in the breathing of auxiliary muscles (abdominal paradox, alternating rhythm - alternation of chest and abdominal breathing types.
Indications for artificial lung ventilation in acute respiratory failure in patients with COPD
Absolute indications:
- respiratory arrest;
- expressed impaired consciousness (stupor, coma);
- unstable hemodynamic disturbances (systolic blood pressure <70 mm Hg, heart rate <50 / min or> 160 / min.);
- fatigue of the respiratory muscles.
Relative indications:
- respiratory rate> 35 / min .;
- severe acidosis (arterial blood pH <7.25) and / or hypercapnia (PaCO2> 60 mmHg);
- RaO2 <45 mm Hg, despite oxygen therapy.
- inefficiency of non-invasive ventilation.
Protocol for the management of patients with exacerbation of COPD in the intensive care unit
1. Assessment of the severity of the condition, radiography of the respiratory system, the gas composition of the blood.
2. Oxygen therapy 2-5 l / min., At least 18 hours / day. and / or non-invasive ventilation.
3. Repeated monitoring of the gas composition after 30 minutes.
4. Bronchodilator therapy:
- Increased dosage and frequency of administration. A solution of ipratropium bromide 0.5 mg (2.0 ml) through a nebulizer with oxygen in combination with solutions of short-acting β2-agonists: salbutamol 5 mg or fenoterol 1.0 mg (1.0 ml) every 2-4 hours.
- The combination of phenoterol and ipratropium bromide (berodual). A solution of berodual 2 ml through a nebulizer with oxygen, every 2-4 hours.
- Intravenous administration of methylxanthines (if ineffective). Eufillin 240 mg / h. up to 960 mg / day. iv with a rate of administration of 0.5 mg / kg / h. under the control of an ECG. The daily dose of aminophylline should not exceed 10 mg / kg of patient body weight.
5. Systemic corticosteroids intravenously or orally. Inside - 0.5 mg / kg / day. (40 mg / day for 10 days), if oral administration is not possible, parenterally up to 3 mg / kg / day. A combined method of prescribing intravenous and oral administration is possible.
6. Antibacterial therapy (with signs of bacterial infection, orally or intravenously).
7. Anticoagulants subcutaneously with polycythemia.
8. Treatment of concomitant diseases (heart failure, cardiac arrhythmias).
9. Non-invasive ventilation.
10. Invasive ventilation (IVL).
Exacerbation of COPD
1. Treatment of exacerbation of COPD on an outpatient basis.
With mild exacerbation, an increase in the dose and / or frequency of taking bronchodilator drugs is indicated:
- Anticholinergics are added (if not previously used). Preference is given to inhaled combined bronchodilators (anticholinergics + short-acting β2-agonists).
- Theophylline - if it is impossible to use inhaled forms of drugs or their insufficient effectiveness.
- Amoxicillin or macrolides (azithromycin, clarithromycin) - with the bacterial nature of exacerbation of COPD.
In case of moderate exacerbation, along with increased bronchodilator therapy, amoxicillin / clavulanate or second generation cephalosporins (cefuroxime axetil) or respiratory fluoroquinolones (levofloxacin, moxifloxacin) are prescribed for at least 10 days.
In parallel with bronchodilator therapy, systemic corticosteroids are prescribed in a daily dose of 0.5 mg / kg / day, but not less than 30 mg of prednisolone per day or other systemic corticosteroids in an equivalent dose for 10 days, followed by cancellation.
2. Treatment of exacerbation of COPD in stationary conditions.
2.1 Oxygen therapy 2-5 l / min, at least 18 hours / day. with the control of the gas composition of the blood after 30 minutes.
2.2 Bronchodilator therapy:
- increase in dosage and frequency of administration; ipratropium bromide solutions - 0.5 mg (2 ml: 40 drops) through a nebulizer with oxygen in combination with solutions of salbutamol (2.5-5.0 mg) or fenoterol - 0.5-1.0 mg (0.5- 1.0 ml: 10-20 drops) - "on demand" or
- a fixed combination of phenoterol and an anticholinergic agent - 2 ml (40 drops) through a nebulizer with oxygen - "on demand".
- intravenous administration of methylxanthines (with inefficiency): aminophylline 240 mg / h to 960 mg / day. iv with a rate of administration of 0.5 mg / kg / h. under the control of an ECG.
2.3 Systemic corticosteroids intravenously or orally. Inside 0.5 mg / kg / day. (40 mg / day. Prednisone or other SCS in an equivalent dose for 10 days), if oral administration is not possible - parenterally up to 3 mg / kg / day.
2.4 Antibacterial therapy (for signs of bacterial infection, orally or intravenously):
2.4.1 Simple (uncomplicated) exacerbation: the drug of choice (one of the following) inside (7-14 days):
- amoxicillin (0.5-1.0 g) 3 p./day ..
Alternative drugs (one of these) inside:
- azithromycin (500 mg) 1 r./day. according to the scheme;
- amoxicillin / clavulanate (625) mg 3 p./day. or (1000 mg) 2 p./day .;
- cefuroxime axetil (750 mg) 2 r./day .;
- clarithromycin CP (500 mg) 1 r./day .;
- clarithromycin (500 mg) 2 p./day .;
- levofloxacin (500 mg) 1 r./day .;
- moxifloxacin (400 mg) 1 r./day.
2.4.2 Complicated exacerbation: the drug of choice and alternative drugs (one of the following):
- amoxicillin / clavulanate 1200 mg 3 p./day .;
- levofloxacin (500 mg) 1 r./day .;
- moxifloxacin (400 mg) 1 r./day ..
If you suspect the presence of Ps. aeruginosa for 10-14 days:
- ciprofloxacin (500 mg) 3 r./day. or
- ceftazidime (2.0 g) 3 r.s.
After iv antibiotic therapy, one of the following drugs is prescribed orally for 10-14 days:
- amoxicillin / clavulanate (625 mg) 3 r./day .;
- levofloxacin (500 mg) 1 r./day .;
- moxifloxacin (400 mg) 1 r./day .;
- ciprofloxacin (400 mg) 2-3 p. / day.
Articles
Forecast
The prognosis for COPD is conditionally unfavorable. The disease slowly, steadily progresses; as it develops, the working capacity of patients is steadily lost.
Continued smoking usually contributes to the progression of airway obstruction, leading to early disability and shortened life expectancy. After quitting smoking, there is a slowdown in the reduction of FEV1 and the progression of the disease. To alleviate the condition, many patients are forced to take drugs in gradually increasing doses until the end of their lives, as well as use additional drugs during exacerbations.
Adequate treatment significantly slows down the development of the disease, up to periods of persistent remission for several years, but does not eliminate the cause of the development of the disease and the formed morphological changes.
Among other diseases, COPD is the fourth leading cause of death in the world. Mortality depends on the presence of concomitant diseases, the patient's age and other factors.
The BODE method (Body mass index, Obstruction, Dyspnea, Exercise - body mass index, obstruction, shortness of breath, physical activity) gives a combined score, which allows predicting subsequent survival better than any of the above indicators taken separately. Studies of the properties of the BODE scale, as a tool for quantifying COPD, are ongoing.
Hospitalization
Indications for hospitalization:
- inefficiency of outpatient treatment;
- increase in hypoxemia;
- the occurrence or increase of hypercapnia;
- the onset or decompensation of the pulmonary heart, not amenable to outpatient treatment.
Hospital discharge criteria:
- the patient is able to take long-acting bronchodilators (β2-agonists and / or anticholinergics) in combination with or without inhaled corticosteroids;
- reception of short-acting inhaled β2-agonists is required no more often than every 4 hours;
- the patient is able (if previously he was on an outpatient care) to independently move around the room;
- the patient is able to eat and can sleep without frequent awakenings due to shortness of breath;
- clinical stability within 12-24 hours;
- stable values of arterial blood gases for 12-24 hours;
- the patient or home care provider fully understands the correct regimen for taking drugs;
- resolved issues of further monitoring of the patient (for example, visits to the patient by a nurse, supply of oxygen and food);
- the patient, the family and the doctor are sure that the patient can be successfully managed in everyday life.
Objects of assessment at the time of discharge from the hospital:
- Confidence in the effectiveness of compliance with the regimen of drug treatment at home;
- re-evaluation of the inhalation technique;
- training on the role of the maintenance treatment regimen;
- instructions for stopping therapy with corticosteroids and antibiotics, if prescribed;
- assessment of the need for long-term oxygen therapy;
- appointment of a second consultation after 4-6 weeks;
- planning for monitoring and treatment of concomitant diseases.
Objects of evaluation during follow-up during a visit 4-6 weeks after discharge from the hospital:
- assessment of the ability to live in a familiar environment;
- the value of FEV1;
- re-evaluation of the inhalation technique;
- assessment of understanding of the recommended treatment regimen;
- reevaluation of the need for prolonged oxygen therapy and / or a home nebulizer;
- the ability to maintain physical and daily activity;
- indicators CAT and mMRC;
- status of concomitant diseases.
Prevention
Specific prophylaxis:
- Quitting smoking.
- Purification of polluted air at the workplace and at home.
Prevention of complications:
- Smoking cessation has a significant impact on the dynamics of COPD (studies on the effects of smoking cessation revealed that 25% of patients succeeded in long-term smoking abstinence).
- Vaccination against influenza and pneumococcal infection.
Information
Patients with COPD, as a rule, are treated on an outpatient basis, without issuing a disability certificate.
Criteria for disability in COPD (Ostronosova N.S., 2009):
- COPD in the acute stage.
- The occurrence or worsening of respiratory failure and heart failure.
- The occurrence of acute complications (acute or chronic respiratory failure, heart failure, pulmonary hypertension, pulmonary heart, secondary polycythemia, pneumonia, spontaneous pneumothorax, pneumomediastinum).
Duration of temporary disability is 10 days or more, and the following factors are taken into account:
- phase and severity of the disease;
- condition of bronchial patency;
- the degree of functional disorders of the respiratory and cardiovascular systems;
- complications;
- nature of work and working conditions.
Criteria for discharge of patients to work:
- improvement of the functional state of the broncho-pulmonary and cardiovascular systems;
- improvement of indicators of exacerbation of the inflammatory process, including laboratory and spirometric, as well as the radiological picture (with joined pneumonia).
Patients are not contraindicated work in office conditions.
Labor factors that negatively affect the health status of patients with COPD:
- adverse weather conditions;
- contact with toxic substances irritating the respiratory tract, allergens, organic and inorganic dust;
- Frequent trips, business trips.
Such patients, in order to prevent recurrence of COPD exacerbations and complications, should be employed at the conclusion of a clinical expert commission (CEC) of the treatment and prevention institution for various periods (1-2 months or more), and in some cases, they should be sent for medical and social examination (ITU).
When referring to a medical and social examination, a limitation of vital activity (moderate, severe or pronounced) is taken into account, associated primarily with impaired respiratory (DNI, DNII, DNIII) and cardiovascular systems (CI, CHII, CHIII), as well as professional history of the patient.
With a mild severity during an exacerbation, the approximate periods of temporary disability in patients with COPD are 10-12 days.
With moderate severity, temporary disability in patients with COPD is 20-21 days.
In severe severity - 21-28 days.
In extremely severe cases - more than 28 days.
Duration of temporary disability is on average up to 35 days, of which inpatient treatment is up to 23 days.
With I degree of DN, shortness of breath in patients occurs with previously available physical efforts and moderate physical stress. Patients indicate shortness of breath and cough, appearing when walking fast, climbing uphill. On examination, mild cyanosis of the lips, tip of the nose, and ears is noted. NPV - 22 breaths per minute; HPF changed slightly; JELL is reduced from 70% to 60%. A slight decrease in the saturation of arterial blood with oxygen from 90% to 80% is noted.
With II degree of respiratory failure (DNII), dyspnea occurs during normal exertion or under the influence of slight physical stress. Patients complain of shortness of breath when walking on level ground, fatigue, cough. Inspection reveals diffuse cyanosis, hypertrophy of the muscles of the neck, taking an auxiliary part in the act of breathing. NPV - up to 26 breaths per minute; a significant change in the HPF is noted; JELL is reduced to 50%. Saturation of arterial blood with oxygen is reduced to 70%.
With the III degree of respiratory failure (DNIII), dyspnea occurs with the slightest physical stress and at rest. Marked cyanosis, hypertrophy of the neck muscles are noted. Pulsation in the epigastric region, swelling of the legs can be detected. NPV - 30 breaths per minute and above. X-ray detect a significant increase in the right heart. FVD indicators are sharply deviated from the proper values; JELL - below 50%. Saturation of arterial blood with oxygen decreases to 60% and below.
The disability of patients with COPD without respiratory failure outside the acute stage is preserved. A wide range of work is available to such patients in favorable conditions.
An extremely severe COPD with an exacerbation rate of 5 times a year is characterized by the severity of clinical, radiological, radionuclide, laboratory and other indicators. Patients have shortness of breath more than 35 breaths per minute, cough with purulent sputum, often in large quantities.
An X-ray examination reveals diffuse pneumosclerosis, pulmonary emphysema, bronchiectasis.
FVD indicators are sharply deviated from normal values, VC - below 50%, FEV1 - less than 40%. Ventilation rates are reduced from the norm. Capillary circulation is reduced.
ECG: marked overload of the right heart, conduction disturbance, blockade more often than the right leg of the bundle of His, a change in the T wave and mixing of the ST segment below the contour, diffuse changes in the myocardium.
As the course of the disease worsens, changes in the biochemical parameters of blood - fibrinogen, prothrombin, transaminase; the number of red blood cells and the content of hemoglobin in the blood due to increased hypoxia; the number of leukocytes increases; the appearance of eosinophilia is possible; ESR increases.
In the presence of complications in patients with COPD with concomitant diseases of the cardiovascular system (coronary heart disease, stage II arterial hypertension, rheumatic heart disease, etc.), neuropsychiatric in-patient treatment, the terms of inpatient treatment are increased to 32 days, and the total duration is up to 40 days.
Patients with rare, short-term exacerbations with DNI need a work device at the conclusion of the KEC. In cases where exemption from the above factors will entail the loss of a qualified profession with constant speech load (singers, lecturers, etc.) and respiratory apparatus tension (glassblowers, brass band musicians, etc.), patients with COPD should be referred to the ITU for the establishment of disability group III by him in connection with a moderate restriction of life (according to the criterion of restricting work activity of the first degree). Such patients are prescribed light physical labor in work conditions not contraindicated and mental work with moderate psycho-emotional stress.
In severe, frequent, prolonged exacerbations of COPD with DNII, CHI or DNII-III, CHIIA, SNIIB, patients should be referred to the ITU to determine their disability group II in connection with a pronounced limitation of life (according to the criteria for limiting the ability to self-care and mobility, II degree and labor activities of the II degree). In some cases, work in specially created conditions, at home, may be recommended.
Significant violations of the respiratory and cardiovascular systems: DNIII in combination with CHIII (decompensated pulmonary heart) determine disability group I due to a pronounced limitation of vital activity (by the criterion of limiting the ability to self-care, mobility - III degree), clinical changes, morphological disorders , a decrease in the function of external respiration and developing hypoxia.
Thus, for the correct assessment of the severity of COPD, the timing of temporary disability, clinical and labor prognosis, effective medical and social rehabilitation, timely comprehensive examination of patients with determination of bronchial obstruction, degree of functional disorders of the respiratory and cardiovascular systems, complications, and concomitant diseases is necessary , nature of work and working conditions.
 DE
DE FR
FR IT
IT ES
ES